Failures in the reprocessing of flexible endoscopes are associated with the development of hospital acquired infections, which subsequently increase the burden on patients and health care systems.1,2,3 These endoscope reprocessing failures can be, in part, attributed to the use of chemical disinfection, which may not always provide the level of decontamination required to protect patients.4-6 As such, there is an increasing need to introduce endoscope sterilization between procedures, as opposed to chemical disinfection, for the prevention of infection in hospitals.1
The Consequences of Inadequate Reprocessing
Hospital acquired infections represent the most reported adverse event affecting patients,1 with a prevalence of 6.5% across Europe.2 These include surgical site infections, comprising 18.3% of all hospital acquired infections,2 which are associated with a negative impact on patient quality of life and increased rates of morbidity and mortality.1, 3 They are also associated with an increased financial burden on health care systems. In Germany, the development of a surgical site infection has been shown to contribute to a prolonged hospitalisation of 17.9 days and increased health care cost of €22,905 per patient.3
Failure to effectively reprocess medical devices can result in instrument contamination and the transmission of microorganisms to subsequent patients. This is highlighted in a report from a Veterans Affairs Medical Centre in Georgia, US, where, because of inadequate adherence to protocols for the reprocessing of medical devices, over 4,600 patients who underwent dentistry, endoscopy, urology, podiatry, optometry and surgical procedures were exposed to human immunodeficiency virus (HIV), hepatitis B and hepatitis C.7 Such exposures have the potential for devastating consequences.
The US Food and Drug Administration (FDA) has shown concern regarding this inadequate reprocessing of medical devices, particularly for duodenoscopes,8 urological endoscopes,9 and bronchoscopes,10 reporting “unacceptably high contamination rates” resulting in infections and deaths.
Duodenoscopes
The FDA received three reports of deaths, 45 reports of patient infection, one report of patient exposure and 159 reports of device contamination between October 2018–March 2019, all of which were attributed to contaminated duodenoscopes. High contamination rates of up to 36.8%, attributed to inadequate reprocessing, have also been reported across multiple studies.11, 12 Contaminated duodenoscopes have the potential to expose patients to a plethora of different microorganisms. This was highlighted in an FDA-ordered post-market surveillance study of Olympus, Fujifilm and Pentax duodenoscopes, which reported that up to 5.4% of samples tested positive for high-concern organisms, including Escherichia coli and Staphylococcus aureus, and 3.6% tested positive for low- to moderate-concern organisms.8
Whilst there is substantial concern regarding potential duodenoscope contamination, it should be noted that other gastrointestinal endoscopes also pose a significant risk of infection. This was noted by a -meta-analysis of 20 studies, which showed that colonoscopes and gastroscopes had a contamination rate of 31.95% and 28.22%, respectively.13
Urological Endoscopes
Between January 2017–February 2021, the FDA received 450 medical device reports describing patient infections or other contaminations with urological endoscopes in the USA, as well as three patient deaths attributed to subsequent bacterial infection.9 This resulted in Karl Storz temporarily recalling over 24 models of urological endoscopes to recommend sterilization only in the Instructions for Use, due to concerns that chemical disinfection would not provide adequate decontamination.14
Contaminated urological endoscopes have the potential to expose patients to pathogenic microorganisms which can lead to the development of urosepsis, a serious complication with reported mortality rates of 20–40% for severe cases.15 A substantial proportion of patients exposed to a contaminated endoscope can go on to develop this complication, with a reported outbreak of Klebsiella pneumoniae caused by use of contaminated ureteroscopes leading to the development of urosepsis in 17 out of 68 exposed patients.16
Bronchoscopes
Between January 2010–June 2015, the FDA received 109 medical device reports worldwide describing patient infection or device contaminations associated with the use of reusable flexible bronchoscopes. This subsequently increased between July 2015–January 2021, with an additional 867 medical device reports received, including seven deaths. The most frequently reported microorganisms were Mycobacterium, Pseudomonas, Serratia and Klebsiella.10
As a result of these reports, the FDA has recommended the use of sterilization instead of chemical disinfection where possible, owing to the higher safety margin provided by sterilization.10
Reasons for Reprocessing Failure
- The reprocessing failures highlighted above can be attributed to several factors, including the failures of chemical disinfectants. There are several reasons why the most adequate method for endoscope decontamination may not be chemical disinfection:
- Chemical disinfection is a lengthy process, where steps can easily be missed.4 There is a need for adherence to guidelines for the decontamination process, which incorporate repeated evaluations of practices and routine examinations.17 However, the pressure for rapid endoscope reprocessing, the difficulty of using test strips to adequately identify the minimum recommended concentration of biocide in each reprocessing cycle, and perceptions of occupational health hazards associated with biocide exposure can contribute to reduced protocol adherence.5
- Chemical disinfection may not provide the microorganism log reduction values required to protect patients, as some microorganisms are more resistant than others.6
- Semi critical medical devices that are typically disinfected may occasionally be used in critical cases.6
- Many endoscopes have complex designs, making them harder to adequately disinfect.4
Alongside inadequate reprocessing with chemical disinfection, irregularities in endoscopic devices can further increase the risk of contamination, despite rigorous cleaning.18 This can lead to an increased likelihood of infection, with one study demonstrating that, out of 104 patients exposed to a damaged, contaminated cystoscope, 11 patients developed a Pseudomonas aeruginosa urinary tract infection.19
An Increased Need for Sterilization
Considering inadequate endoscope reprocessing using chemical disinfectants, exacerbated by micro-damages on devices, there is an increasing need to adopt flexible endoscope sterilization in health care practice. Medical equipment sterilization has a higher margin of safety than disinfection as the process results in complete destruction of all pathogenic microorganisms, whereas disinfection destroys most, but not all, microbial forms.1 The use of sterilization aligns with the FDA recommendations for the reprocessing of flexible bronchoscopes as well as the recommendation from Advanced Sterilization Products (ASP): What can be sterilized - should be sterilized.
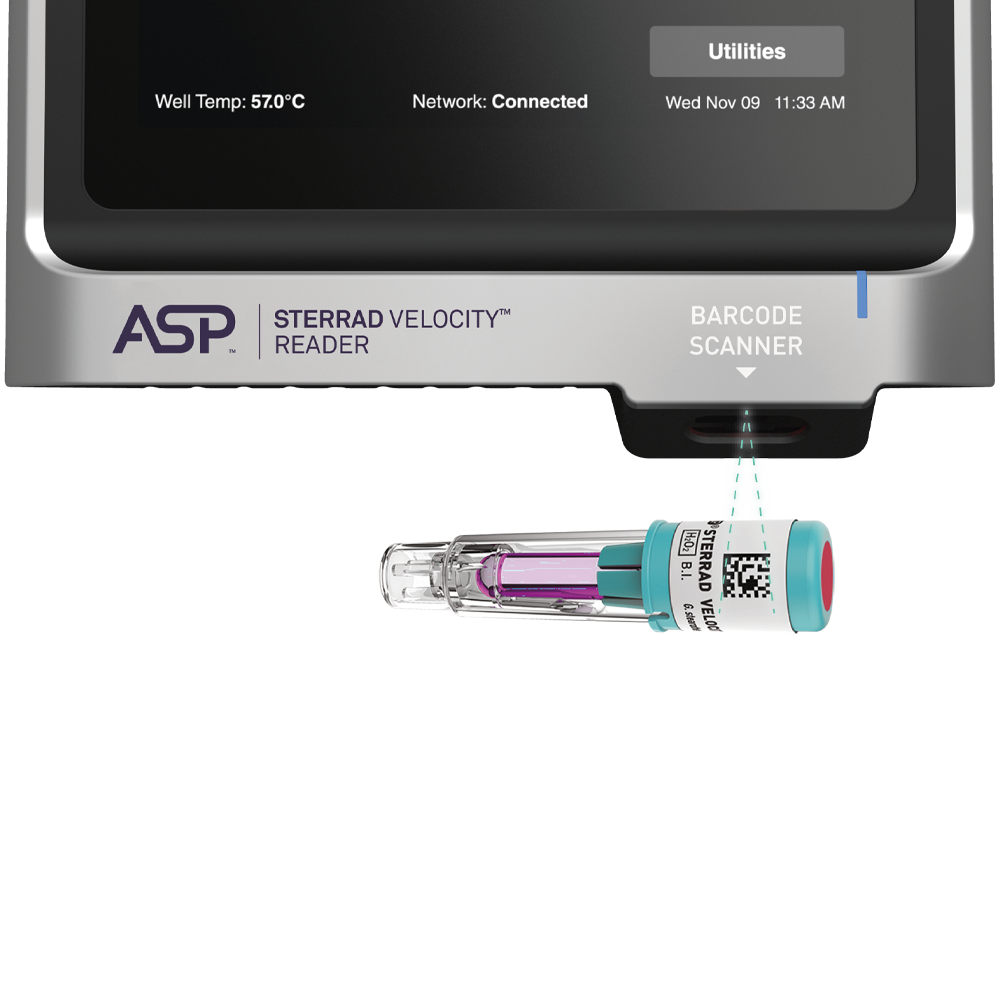
Low temperature hydrogen peroxide sterilization in ASP STERRAD™ Systems ensures adequate decontamination of endoscopes, minimising the risk of patient exposure to infection20. To provide further confidence in the effectiveness of these sterilization cycles, the STERRAD VELOCITY™ Biological Indicator/Process Challenge Device (PCD) also monitors and tests sterilization by providing a challenge greater than or equal to the most challenging medical device indicated for reprocessing. These tests provide sterility assurance by confirming that a cycle has successfully inactivated microorganisms.21
References
Global guidelines for the prevention of surgical site infection, second edition. Geneva: World Health Organization; 2018. Licence: CC BY-NC-SA 3.0 IGO.
Suetens C, Latour K, Kärki T, et al. Prevalence of healthcare-associated infections, estimated incidence and composite antimicrobial resistance index in acute care hospitals and long-term care facilities: results from two European point prevalence surveys, 2016 to 2017. Euro Surveill 2018;23.
Badia JM, Casey AL, Petrosillo N, et al. Impact of surgical site infection on healthcare costs and patient outcomes: a systematic review in six European countries. J Hosp Infect 2017;96:1-15.
Hildebrand EA, Branaghan RJ, Neuman BL, et al. An Expert Perspective of Errors in Endoscope Reprocessing. Proceedings of the Human Factors and Ergonomics Society Annual Meeting 2011;55:748-752.
Ofstead CL, Hopkins KM, Buro BL, et al. Challenges in achieving effective high-level disinfection in endoscope reprocessing. Am J Infect Control 2020;48:309-315.
Rutala WA, Kanamori H, Sickbert-Bennett EE, et al. What's new in reprocessing endoscopes: Are we going to ensure "the needs of the patient come first" by shifting from disinfection to sterilization? Am J Infect Control 2019;47s:A62-a66.
Dyer, J. Veterans Potentially Exposed to HIV, HCV at Georgia Hospital. 2022. Available from: https://www.mdedge.com/fedprac/article/252523/hiv/veterans-potentially-exposed-hiv-hcv-georgia-hospital. Accessed 16/01/2023.
Brooks, M. Duodenoscope Contamination Rates Still Lethally High: FDA. 2019. Available from: https://www.medscape.com/viewarticle/911756. Accessed 16/01/2023.
U.S. Food and Drug Administration. FDA is Investigating Reports of Infections Associated with Reprocessed Urological Endoscopes. 2021. Available from: https://www.fda.gov/news-events/press-announcements/fda-investigating-reports-infections-associated-reprocessed-urological-endoscopes. Accessed 16/01/2023.
U.S. Food and Drug Administration. Flexible Bronchoscopes and Updated Recommendations for Reprocessing: FDA Safety Communication. 2021. Available from: https://www.fda.gov/medical-devices/safety-communications/flexible-bronchoscopes-and-updated-recommendations-reprocessing-fda-safety-communication. Accessed 16/01/2023.
Okamoto N, Sczaniecka A, Hirano M, et al. A prospective, multicenter, clinical study of duodenoscope contamination after reprocessing. Infect Control Hosp Epidemiol 2022;43:1901-1909.
Casini B, Spagnolo AM, Sartini M, et al. Microbiological surveillance post-reprocessing of flexible endoscopes used in digestive endoscopy: a national study. J Hosp Infect 2023;131:139-147.
Goyal H, Larsen S, Perisetti A, et al. Gastrointestinal endoscope contamination rates - elevators are not only to blame: a systematic review and meta-analysis. Endosc Int Open 2022;10:E840-e853.
Marcus, A. Urologic Scopes Recalled Over Contamination Fears. 2022. Available from: https://www.medscape.com/viewarticle/971555. Accessed 16/01/2023.
Dreger NM, Degener S, Ahmad-Nejad P, et al. Urosepsis--Etiology, Diagnosis, and Treatment. Dtsch Arztebl Int 2015;112:837-47; quiz 848.
Güler Y, Erbin A, Gozdas T. An outbreak of postoperative rapidly developing and multidrug-resistant Klebsiella pneumoniae urosepsis due to a contaminated ureteroscope. Folia Med (Plovdiv) 2022;64:401-407.
Scotland KB, Lange D. Prevention and management of urosepsis triggered by ureteroscopy. Res Rep Urol 2018;10:43-49.
Ofstead CL, Wetzler HP, Heymann OL, et al. Longitudinal assessment of reprocessing effectiveness for colonoscopes and gastroscopes: Results of visual inspections, biochemical markers, and microbial cultures. Am J Infect Control 2017;45:e26-e33.
Sorbets E, Evrevin M, Jumas-Bilak E, et al. An outbreak of Pseudomonas aeruginosa urinary tract infections following outpatient flexible cystoscopy. Am J Infect Control 2019;47:1510-1512.
Rutala WA, Gergen MF, Sickbert-Bennett EE, et al. Comparative evaluation of the microbicidal activity of low-temperature sterilization technologies to steam sterilization. Infect Control Hosp Epidemiol 2020;41:391-395.
Advanced Sterilization Products. STERRAD VELOCITY™ Biological Indicator/Process Challenge Device. Available from: https://www.asp.com/sites/default/files/pdf/Velocity/STERRAD%20Velocity%20PCD%20Brochure.pdf. Accessed 30/01/2023.